In middle age, you, as a man, or your sexual partner (keeping this observation to her/himself), will likely start to notice a group of symptoms due to a slow but inevitable decline of your male hormone testosterone. As the movie director Martin Scorsese put it well, “Sex becomes memory.” Not necessarily. Not by a long shot.
The medical term for this hormonal mischief is “andropause” sometimes called “male menopause.” I see billboards along the expressways referring to “low T.”
In case you’re young enough, or oblivious enough never to have noticed anything amiss, here are some symptoms you might experience down the
“Long Lonesome Low T Road,” trails of which vary among men themselves
You know for certain that pressing urgency you once had for sex(a/k/a your libido) is steadily declining. The “stirring” isn’t there like it used to be. This is not the same as your new disappointment in your erection. That’s a different department altogether usually quickly repaired with Viagra or Cialis, neither of which do anything for libido. In the privacy of your bedroom, you look in the mirror and you see your body is changing. Despite your best intentions at the health club, your muscles are flabby, you’re getting a potbelly, you’ve lost a lot of your scalp, pubic and armpit hair and (Heaven forfend!) your genitals look smaller! And the amount of sperm you’re shooting out? Don’t even ask!
You might feel grumpier and impatient, depressed, less creative, have minor problems with memory (like word finding, or not remembering a name), and experience some insomnia.
And then there’s the chronic tiredness. With what once was a normal day’s activity, you now want to stay in bed longer, have an afternoon nap, go to bed earlier, fall asleep while watching TV.
As one patient described it well “My get-up-and-go-just-got-up-and-went.”
Causes Of Low T
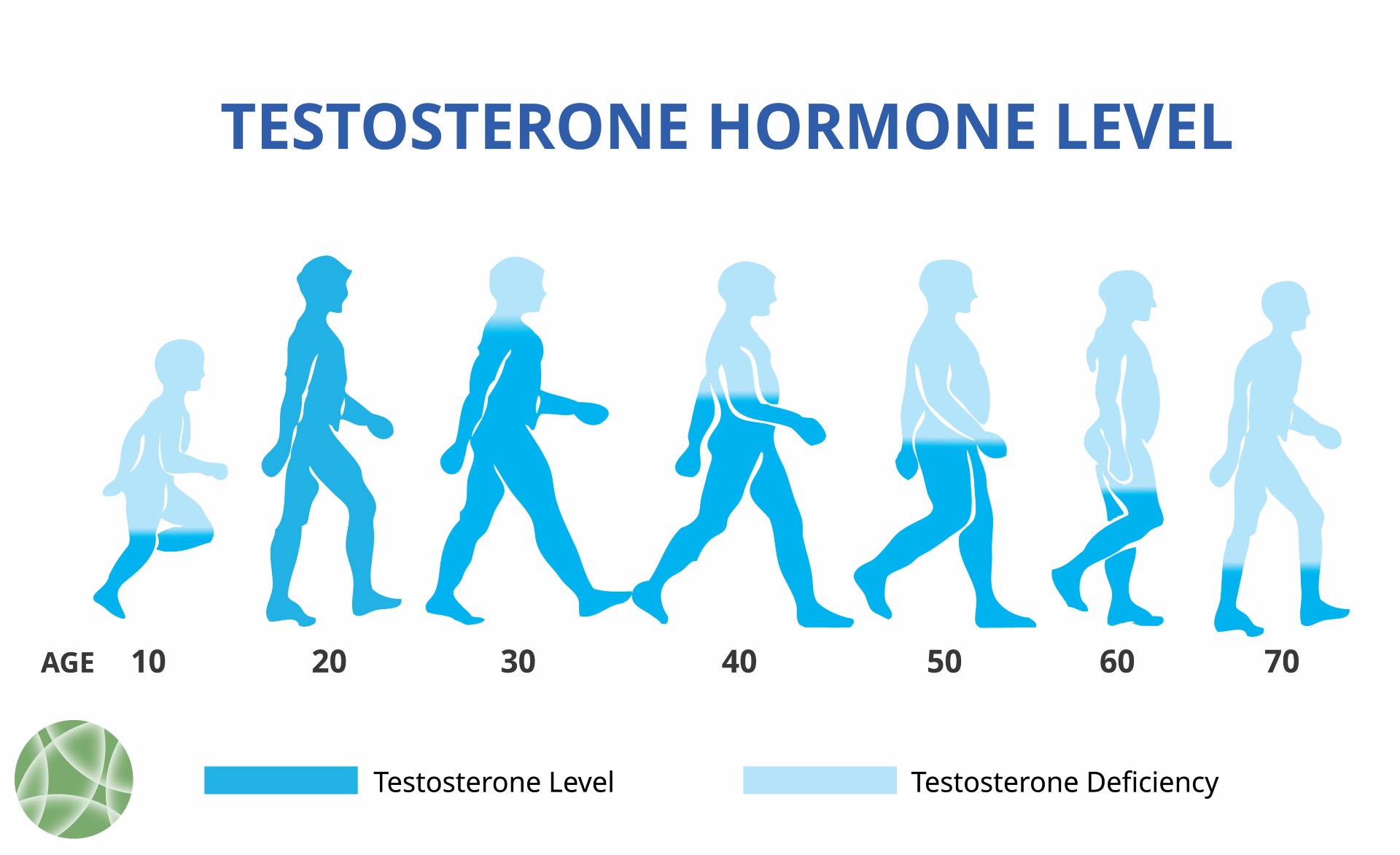
The usual cause of Low T is simply the passage of time and, in fact, your testosterone level will drop by 1% every year starting at AGE 30. And, unfortunately, a variety of medical conditions can speed this along:
- Chemotherapy
- Obesity
- Medication complications, side effects, or drug abuse
- Diabetes
- Hypothyroidism
- Trauma
- Injury of the testes, metabolic disorders
- Excessive estrogen production from your testes
- Alcohol abuse
Testosterone myths
It’s useful to clear the air about testosterone myths and half-truths, especially if you’re a man with symptoms or you’re living with a guy who’s beginning to get on your nerves.
Myth #1: heart disease There was a large kerfuffle with much publicity after a 2013 study published in JAMA reported increased heart disease risks among testosterone users. Days after the study was published, readers and researchers wrote letters pointing out that the study’s arithmetic was faulty. JAMA published a new version, this time with the correct math, which showed that heart disease risk was reduced by 50% among men using testosterone.
The latest research is now showing that:
- Low testosterone is linked to increased coronary artery disease and that when testosterone levels are restored to normal, cardiovascular disease deaths are reduced by 50%.
- Exercise capacity among men with known heart disease who are taking testosterone is much better than among men receiving a placebo.
- There is uniform improvement in heart disease risk factors (fat mass, waist circumference, pre-diabetes indicators) among men taking testosterone vs. placebo.
Myth #2: prostate cancer Just as the Women’s Health Initiative years ago incorrectly concluded that hormone replacement therapy caused breast cancer (it does not), the myth that testosterone replacement causes prostate cancer (it does not) has hung on. Based on what turned out to be a single opinion about one patient, it has never been confirmed in long-term studies using large numbers of patients. What is true is that sex hormones–whether estrogen for women or testosterone for men–can hasten the growth of existing breast and prostate cancers.
This is why women are screened with a mammogram and men with a PSA (prostate-specific antigen) test before being prescribed hormones. The PSA test can be useful as a baseline when tracking testosterone use. If it starts out normal and suddenly shoots skyward with testosterone, the testosterone is stopped.
Myth #3: T is overprescribed because of pharmaceutical advertising Actually, the opposite is true. Levels aren’t measured during routine exams and testing is virtually never suggested by primary care physicians. Too many doctors, their brains hard-wired into the faulty testosterone/heart risk association, discourage both testing and prescribing. In addition, because testosterone is seriously overpriced, insurance companies make every effort to deny coverage. Many insurance companies actually request your testosterone test results to verify that your level is low enough to merit a prescription.
If anything, in my view, testosterone is vastly under-utilized. A lot of men are missing out on a valuable therapy that has the potential to benefit their overall quality of life and reduce some significant health risks.
Testosterone and Longevity
Since this has been part of a series on Longevity Medicine, the most interesting new developments in restoring testosterone to healthy levels is how doing so will effect your longevity. Several articles have appeared during the past few years analyzing the data of men receiving testosterone therapy and have found improvement of lifespan of 5-10%. This has been attributed to a variety of factors: better energy means better ability to exercise and improved heart health, better overall sense of well being, improved sleep.
Additional Important Testosterone Facts
Without insurance (or when insurance denies coverage) Big Pharma testosterone averages $500 a month. Generic options are now available but there is no (repeat ‘no,’ clinical testing done on these products.
The Big Pharma Products are all 50 mg/ml (read this as “one-size-fits-all”). Many men need a stronger product.
Compounding pharmacies will make you testosterone cream based on your personal need and can adjust your dose concentration based on blood tests. The out-of-pocket price is about $75 a month When you receive your “T” treatment at WholeHealth Chicago, we will also monitor your testosterone levels, PSA (prostate), your blood count, and if the testosterone levels are not to our mutual satisfaction, suggest testosterone injections and/or peptide therapies.
Simultaneous Anti-Aging Infusions
Although not required for successful treatment of low testosterone, you should consider twice monthly adding on Anti-Aging Infusions. The most popular is this.
If you want to start work on your steadily declining testosterone, call and schedule with any of our practitioners
Be well,
David Edelberg, MD