Did you ever wonder why some obese people, after decades of being badgered by their families and physicians to lose weight, out-live all of them and are healthy for decades? Or how someone of normal weight falls over dead in his fifties from a massive heart attack the week after his check-up which included a perfect cholesterol?
Here begins chronic inflammation
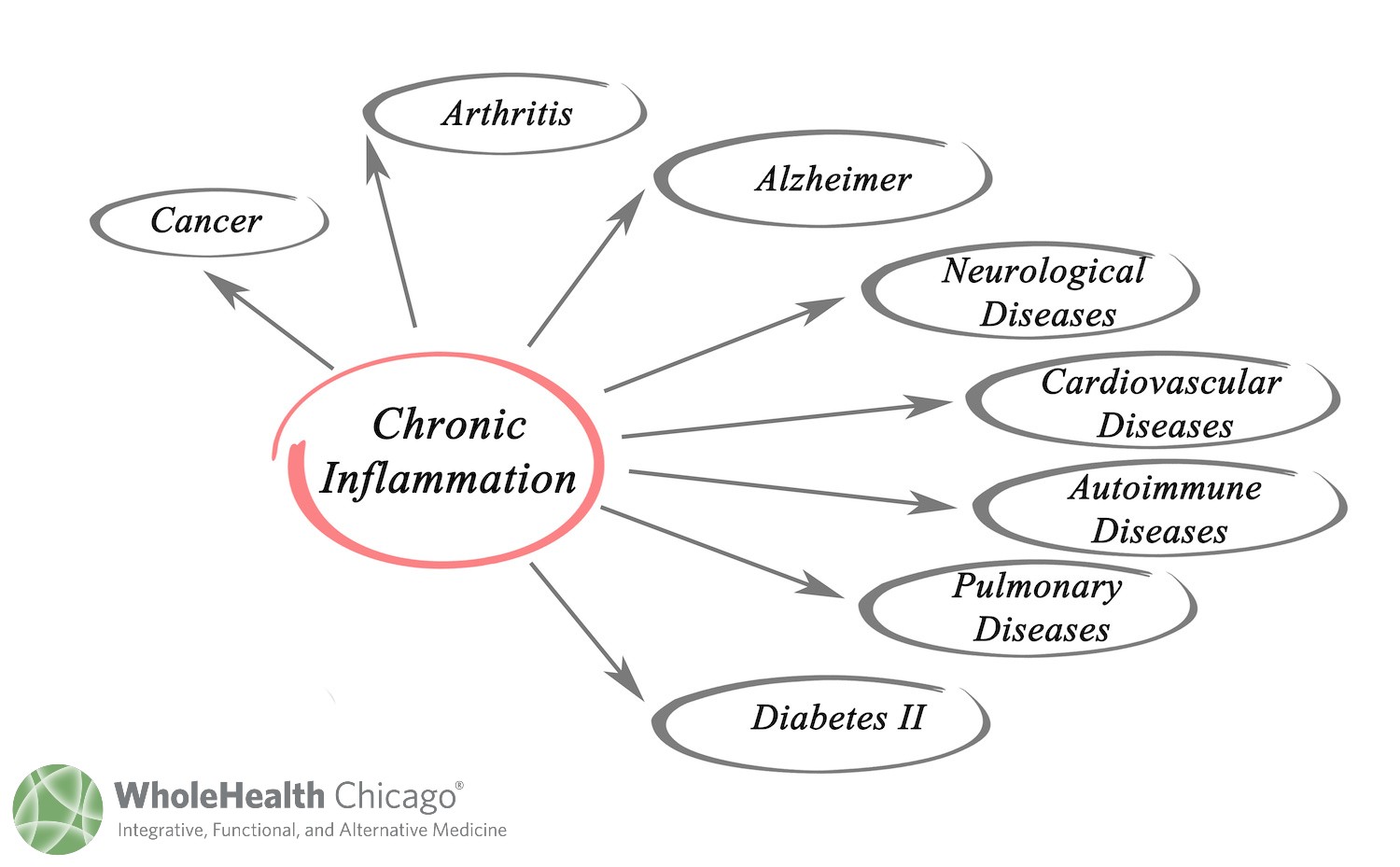
This apparent injustice is not the devil’s work but something else associated with Satan—fire, or rather inflammation. Clues about chronic smoldering inflammation as a basis of disease began to appear some years ago when it was discovered there was a connection between seemingly unrelated illnesses related to premature aging. The list included heart disease, diabetes, the full spectrum of autoimmune diseases, and even dementia, schizophrenia, and Down’s syndrome.
Blood tests for chronic inflammation, most commonly the sedimentation rate (“sed rate”), high sensitivity C-Reactive Protein (“hsCRP”), and ferritin, had been available for decades, but because of these associated diseases, began to appear on routine annual physical examinations or get requested by patients themselves. When confronted with abnormal results, some doctors suggested aspirin, others curcumin, still others didn’t exactly know what to do with the test result and referred patients to various specialists.
There is one “good guy”: acute inflammation saves your life
Your body mounting what’s called an acute inflammatory response is a good thing…when you need it. And you need it to ward off any invader, whether it’s strep bacteria on your tonsils or a splinter in your thumb. During an acute response, a truly elegant radar system triggers the release of key chemicals just when and where they’re needed. The chemicals signal your blood to send troops of white blood cells to kill bacteria plus enzymes to clean up the battlefield. When you had that splinter, your thumb became swollen and red. That was an acute inflammatory immune response, and it’s a beautiful thing. Otherwise the splinter could kill you. It’s called ‘blood poisoning’.
However, picture your body’s acute inflammatory response coming with a label that reads, “for emergency use only”.
And now, in addition to the troubles of chronic inflammation, it’s time for “pro-inflammatory cytokines”.
Pro-inflammatory cytokines, and there are many of them, are a specific type of molecule that starts to appear when one level of acute inflammation is going on and suddenly the body thinks it needs “more”. Unfortunately, as doctors learned from the COVID-19 pandemic, the system can easily spin out of control (remember the words “cytokine storm”?) because these cytokines can cause massive tissue injury, especially pneumonia, and now leave us with long COVID symptoms. We’re now fairly certain that elevations of pro-inflammatory cytokines are also responsible for the muscle pain of fibromyalgia, the inflammation of black mold exposure, and possibly even Alzheimer’s disease.
Unfortunately, at this point, we have not answered the “why” of cytokine release. Why do some people have high levels of cytokines and suffer the pain of fibromyalgia and others don’t. Why do some people when exposed to the toxins of black mold develop CIRS (“chronic inflammatory response syndrome”) from cytokines and others don’t. Why do some people get long COVID and other brush their COVID off like a bad cold?
So that when the news story was released last month, how a serious bout of long COVID had the effect on a brain of 20+ years of aging, you can see the connection with brain inflammation and pro-inflammatory cytokines.
With chronic inflammation (inflama is Latin for “inflame” or “ignite”), your body is literally smoldering, cooking itself. Unfortunately, you don’t have much of a warning system that chronic inflammation is festering in your body, though some people are more sensitive to it than others. When my patients try to describe it, it’s really vague, like “I don’t know, doctor, something’s wrong, I feel inflamed.”
Other patients feel fine, and when they come in for a check-up have nothing to report. But slowly, over the years, this same person will develop conditions linked with chronic inflammation: high blood pressure, heart disease, diabetes, joint inflammation, digestive symptoms like reflux or colitis, and even dementia and cancers.
It is now simply accepted as fact that healthy aging is impaired in people who had been diagnosed as chronically inflamed, indicated by high levels the inflammatory markers (sed rate, hsCRP, ferritin). These markers are molecules circulating in your bloodstream that reflect increased inflammation.
I’ve already mentioned the oldest of these markers, the sed rate (ESR, or erythrocyte sedimentation rate) and C-Reactive Protein (CRP). Others include ferritin, fibrinogen, interleukin-6 (IL-6), and adiponectin and C4a. By tracing just one of these markers–IL-6–investigators noted that individuals with high levels aged poorly, developing many chronic illnesses and dying prematurely. The statement from one group of the investigators sums it up: high inflammation equals “decreased likelihood for successful aging”, and “favorable inflammatory status is positively associated with metabolic health in obese and non-obese subjects”. But really, if any of these is constantly elevated, it does mean your immune system is in overdrive, working to fight or clear away “something”, sometimes known, like COVID-19, sometimes unknown, as is the situation with autoimmune diseases.
Here’s one important point about that list of chronic diseases associated with inflammation, such as the autoimmune spectrum, Alzheimer’s, Parkinsonism, schizophrenia and so forth.
If you have a family member with one of these conditions, don’t be afraid to ask the doctor managing the case if he/she is exploring possibilities of chronic inflammation and if he/she is willing to start anti-inflammatories like low dose naltrexone, dietary changes, and nutritional supplements. If not, then why not, especially when nothing else has been shown to be effective.
What I’ve learned is that many times these interesting treatments are blocked by “committee” and your doctor has no choice but to abide but to abide by “committee decision”. Too bad for your Dad.
How can I tell if I’m inflamed?
Well, unless you get tested, you really don’t know for sure. However, if you’re living an unhealthful lifestyle, odds are that you’re chronically inflamed. Also, regardless of your age, if you’ve got more symptoms (aches and pains, digestive, respiratory, fatigue) or are taking more medicines than friends your own age, you should probably get tested for inflammatory markers. People who have a medicine chest filled with steroid skin creams, asthma inhalers, Nexium-type meds to reduce acid, and NSAIDs for body aches are also likely chronically inflamed.
When it comes to chronic inflammation, lifestyle choices are highly influential. You’re increasing the level of inflammation in your body if:
- You smoke;
- You don’t exercise regularly;
- You eat a nutritionally poor diet rife with refined flour, sugar, animal fats, and processed foods filled with additives, chemicals, and preservatives;
- You’re stressed out;
- You’ve got some hidden food sensitivities (gluten is a big villain here);
- You have chronic, low-level infections from bacteria, parasites, candida, or viruses;
- Your teeth are in bad shape, and you don’t floss (dental plaque is a constant source of inflammation);
- You have chronically inflamed skin that constantly requires steroid creams to reduce its redness.
How can you test for inflammation in your body?
The simplest blood tests to order to assess the inflammatory status are the high-sensitivity C-reactive protein (hsCRP) and the sed rate, virtually always covered by your insurance.
What can you do to minimize inflammation?
Just do the opposite of everything listed in the unhealthful bullet points:
- Eat a nutritious diet of whole foods with plenty of fresh fruits and vegetables (which themselves are anti-inflammatories). Avoid processed foods, refined-flour products (this list is enormous, including most breads, pastas, cookies, cakes, and pies), and sugar (ditto the enormous list). Go gluten-free for a couple weeks and if you feel a lot of your chronic symptoms disappear, only to return when you re-introduce gluten, best stay off it forever. If you need help, schedule with Becca, our nutritionist, to guide you through our low inflammation nutrition program.
- Eat more fish for their omega 3s and switch to healthy fats like olive oil.
- Exercise regularly. This alone can lower your inflammatory markers.
- Reduce stress. Learn meditation, do yoga, avoid being an overworked and unhappy anything (doctor, lawyer, teacher, corporate player) in some huge system where you have no control of your life. I think Somali pirates have less stressful jobs than many of my patients.
- Stop smoking (I can’t believe I still have to tell people to do this).
- Get your teeth cleaned and fixed. Then brush and floss them every day.
- If you have any condition associated with chronic inflammation, read about Low Dose Naltrexone. Discuss it with your personal physician or your WholeHealth Chicago practitioner. It works by regulating your immune system. I have written about LDN here.
- Helpful supplements include a probiotic to heal the lining of your intestines. Take the following natural anti-inflammatories twice a day:
Theracurmin HP (Integrative Therpeutics)
SPM Active (Metagenics) very high potency omega-3
Resveratrol (Integrative Therapeutics)
All right, get started. Put the smoldering fires out.
Be well,
David Edelberg, MD